Enhance your Goal Attainment Scaling Knowledge, from Setting Meaningful Goals to Measuring Success.
Goal Attainment Scaling (GAS) is an individualized patient-centered outcome that quantifies the effects of an intervention based on personal goals. Patients, caregivers, and healthcare professionals work together to identify and set treatment goals that area meaningful to them.
Since its introduction in 1968 by Kiresuk and Sherman1, Goal attainment scaling (GAS) has been a reliable and highly responsive measure of meaningful changes. Over 160 clinical trials have recorded GAS as an outcome, and it has been shown to be responsive to interventions in several disciplines.2
The use of GAS aligns with the FDA's Patient-Focused Drug Development: Incorporating Clinical Outcome Assessments Into Endpoints for Regulatory Decision-Making Draft Guidance #4, which highlights GAS as one of several useful personalized endpoints that can be used to reflect what is important for each patient in clinical trials specifically for diseases with variable clinical manifestations and impact on multiple aspects of feeling and functioning.3
Goal Attainment Scaling focuses on what matters most to the subject and their family.
Clinician to facilitate interview for the patient or caregiver to identify goals.
Together, they set the 5-point goal attainment scale for each identified goal.
Both rate during follow-up whether the goals have been attained.
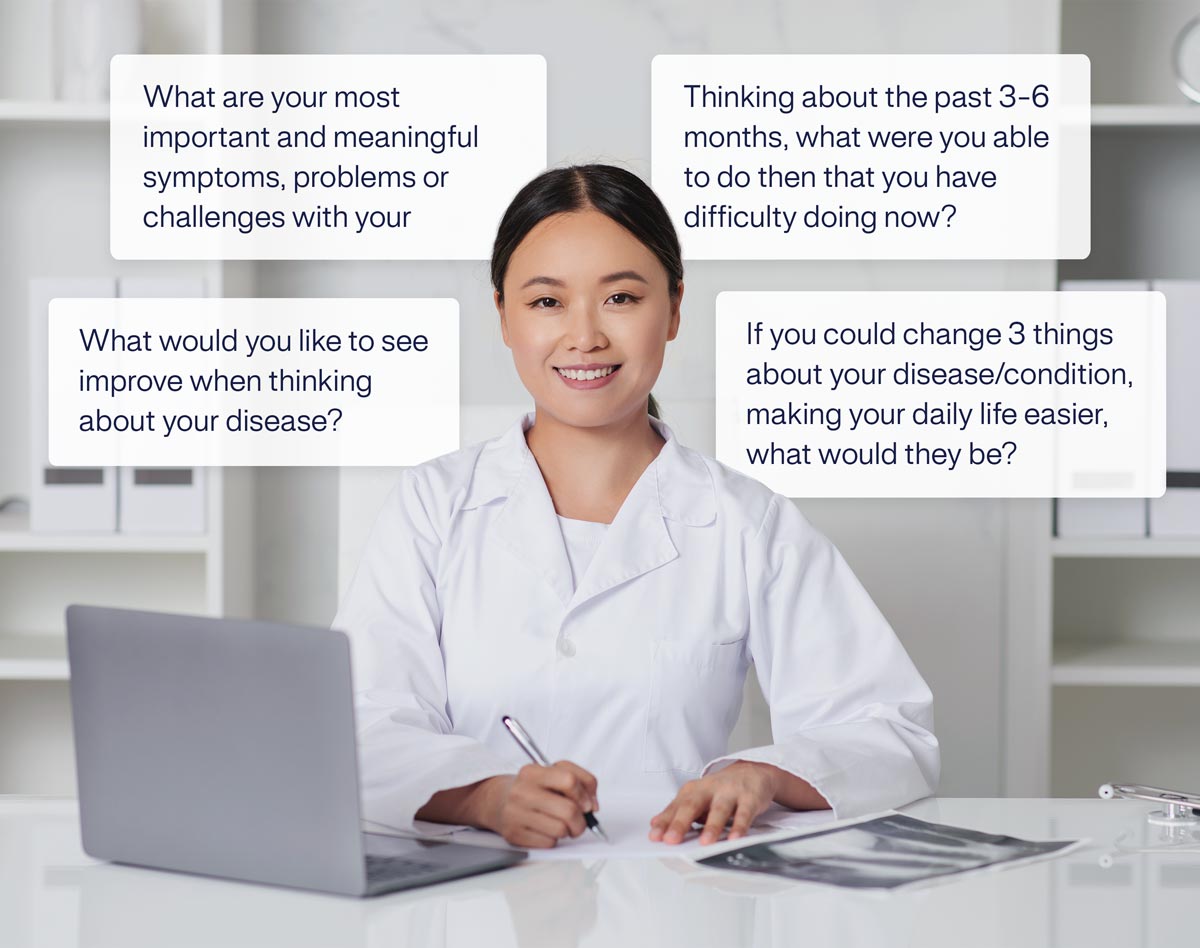
The GAS interviewer (healthcare professional) and the patient (and/or caregiver) work together to identify goals that matter most for the subject before the intervention begins. Patients are asked to identify at least 3 goal areas that are important to them and they would like to see improved by treatment.
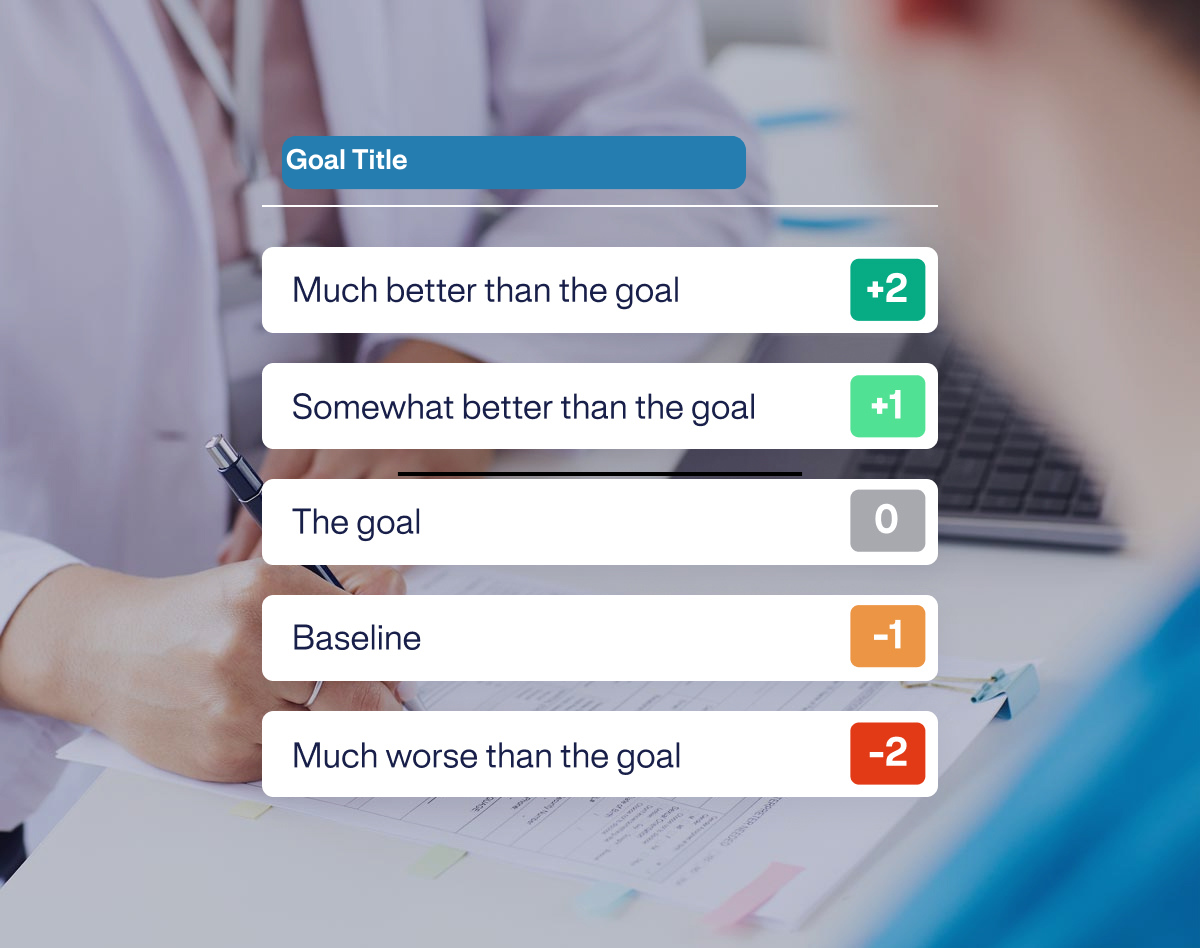
Once goal areas are identified, the patient describes their current state (baseline set at the -1 level on the scale) for each. Then, the GAS interviewer and the patient work together to specify the goal level and identify what improvement would look like (set at 0 level on the scale). The other attainment levels for better and worse outcomes are also identified, and a 5-point scale is developed for each goal area.
The GAS interviewer uses their clinical expertise to facilitate the goal-setting interview and ensure goals are SMART (Specific, Measurable, Achievable, Realistic/Relevant to the intervention, Time-bound).
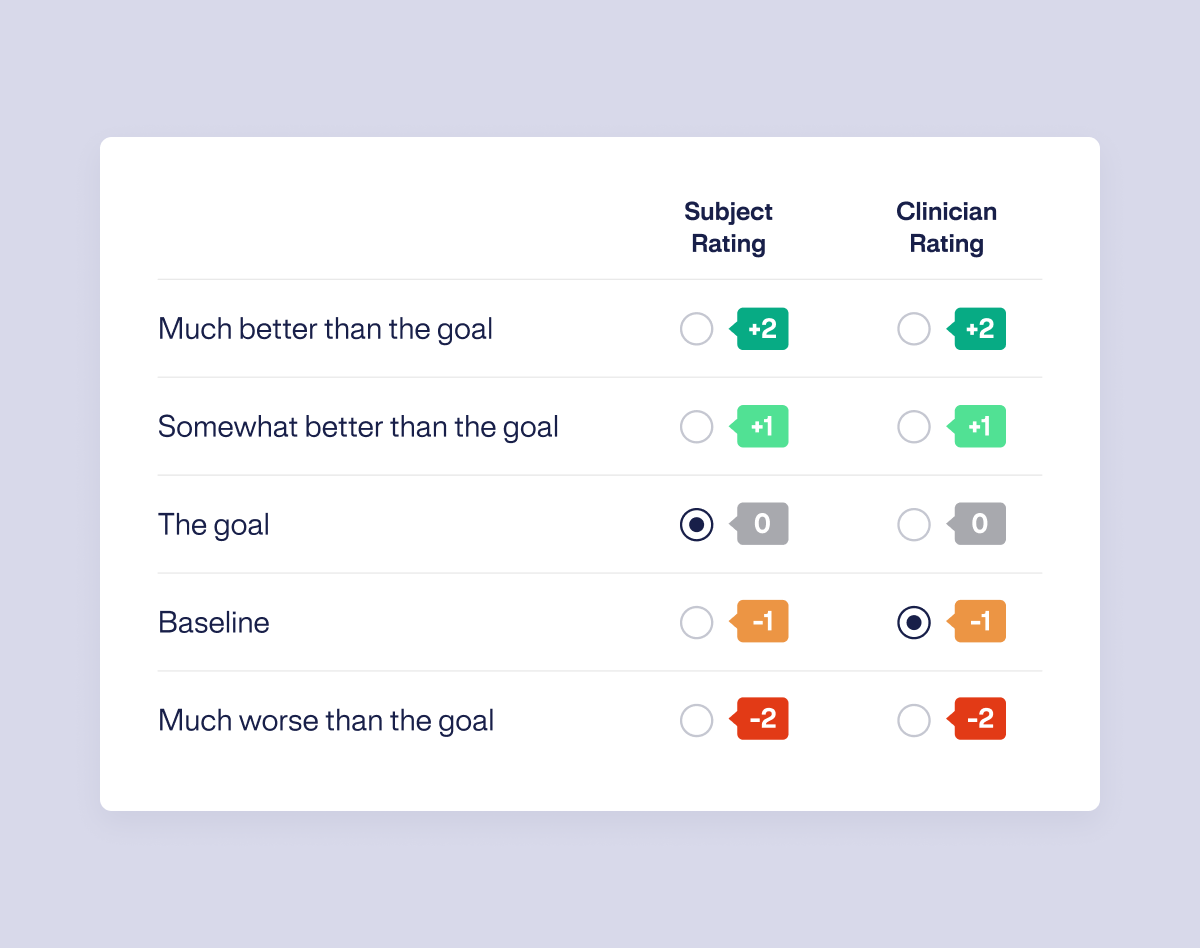
At each predetermined follow-up visit, goal attainment is assessed. Patients are asked to describe their current state in relation to each goal area. The 5-point scale is reviewed together, and the patient is asked to rate their level of attainment. The GAS interviewer will also record their impression of attainment for each goal, which need not be the same as the participant’s rating.
For each participant, a summary score reveals the extent to which goals have been attained. The goals can be ranked by difficulty and importance. The scoring formula corrects for differential weighting of goals and differing number of goals between patients.